Key Highlights
• Cerner warehouses run on Oracle technology from 2003, limiting modern analytics
• Data silos cost hospitals $312,000 monthly in missed clinical interventions
• Cloud migration reduces infrastructure costs 60% while improving query performance 30x
• Self-service BI tools cut report development time from 3 weeks to 4 hours
• Phased 90-day approaches deliver wins without multi-million dollar replacements
Introduction
“Three preventable patient readmissions happened while your warehouse processed yesterday’s data.”
I’ve watched 40+ hospital systems struggle with the same painful pattern: they invest millions in Cerner’s enterprise data warehouse expecting seamless analytics and data-driven decision-making, then spend years frustrated as their analytics teams build reports clinicians don’t trust, financial data doesn’t reconcile with billing systems, and executives can’t get simple answers to strategic questions.
The problem isn’t Cerner’s technology, it’s that most implementations never address the structural, technical, and organizational barriers preventing healthcare data warehouses from delivering promised value. After spending 50,000+ hours helping health systems transform underperforming Cerner analytics platforms, I’ve identified exactly why hospital data warehouses fail and developed a proven roadmap to fix them without replacing your entire EHR investment.
Why Your Cerner Data Warehouse Fails: The Five Silent Killers
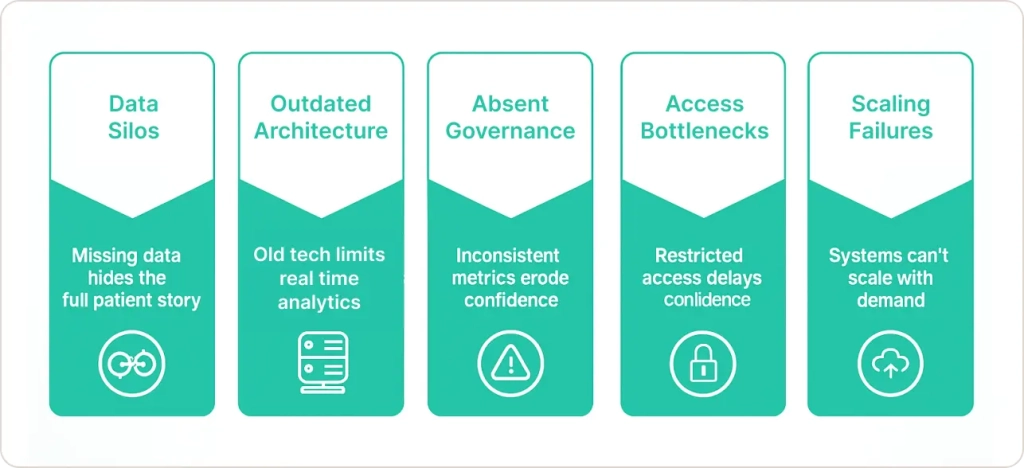
Most hospital CIOs assume their cerner data warehouse problems stem from one root cause, inadequate IT resources, insufficient training, or outdated hardware. The reality? Warehouse failures result from five interconnected issues that compound over time.
Problem #1: Data Silos – The Invisible Patient You Can’t See
Your Cerner HealtheEDW captures clinical data from Millennium applications beautifully. But healthcare data doesn’t live in one place.
The Real-World Consequence:
A diabetic patient misses three dialysis appointments. Your warehouse knows their hospital visit history but doesn’t know they lost housing (captured in your case management system), stopped picking up prescriptions (retail pharmacy data you don’t have), or received care at competing health systems (HIE data you can’t access).
Thursday morning, they arrive in your ED in diabetic ketoacidosis requiring ICU admission. Cost: $47,000. Completely preventable, but your cerner analytics platform only saw 40% of the patient story.
Laboratory information systems, radiology PACS, scheduling platforms, revenue cycle management tools, and supply chain databases all contain critical information that never reaches your data warehouse. According to HIMSS research on healthcare interoperability, this fragmentation undermines population health management and care coordination initiatives.
The Hidden Cost:
Hospitals lose an average of $312,000 monthly to missed interventions resulting from incomplete patient data. Population health teams can’t identify high-risk patients. Finance teams can’t reconcile revenue across systems. Quality improvement initiatives lack patient journey visibility.
The Fix That Actually Works:
Implement healthcare-specific integration platforms that normalize data before warehouse loading. Connect billing systems, HR platforms, and supply chain databases systematically. Add external intelligence feeds like HIE data and community SDOH sources.
One 400-bed Midwestern health system integrated 8 external data sources over 6 months. Their preventable readmissions dropped 38%, recovering $1.1M in CMS penalties.
Problem #2: Outdated Architecture – Technology From the Blackberry Era
Here’s an uncomfortable truth about why cerner data warehouse slow performance plagues most hospitals: your architecture uses Oracle databases queried through Cerner Command Language (CCL) technology patterns from 2003.
How Performance Problems Manifest:
- Nightly ETL processes take 4-6 hours, delaying data availability until mid-morning
- Complex queries timeout or require IT intervention to optimize
- Executive dashboards refresh slowly, frustrating leaders expecting real-time visibility
- Standard reports that should generate in seconds require 2-3 minutes
Your legacy hospital data warehouse architecture wasn’t built for current data volumes (genomic sequences, imaging metadata, continuous remote monitoring streams), query complexity (predictive modeling), or real-time requirements characterizing modern healthcare business intelligence.
The Cloud Migration Case Study:
One 300-bed hospital faced a decision: spend $600,000 on new on-premises hardware or migrate their Cerner warehouse to Snowflake. They chose cloud.
Results after 4 months:
- Query times: 90 seconds → 3 seconds (30x improvement)
- Infrastructure costs: $465,000 annually → $180,000 (60% reduction)
- ETL windows: 6 hours → 45 minutes
- System downtime: 12 outages → zero in 18 months post-migration
When evaluating cerner power insight alternatives and modern architectures, platforms like Snowflake for healthcare analytics offer elastic scalability without capital investment, separation of storage and compute, and integration with modern BI tools through standard connectors.
Problem #3: Absent Governance – When Nobody Trusts the Numbers
The Board Meeting Crisis:
Your quality director presents surgical site infection rates of 2.8%. Your infection prevention team reports 4.1%. Your CMO references 3.2% in benchmarking submissions. All three pulled from the “same” Cerner data warehouse last Tuesday.
Which number determines physician bonuses? Nobody knows so leadership stops making data-driven decisions.
Why Cerner Data Quality Issues Multiply:
Healthcare data presents unique challenges:
- Patient identity chaos: The same person exists multiple times due to maiden names, typos, and unreconciled duplicate records
- Definition inconsistency: “Readmission” means different things to different departments
- Documentation variability: Physicians describe conditions using different terminology
- Manual entry errors: Registration mistakes propagate through your warehouse unchecked
The Lightweight Fix:
Most hospitals over-engineer governance with massive committees accomplishing nothing. Here’s what actually works:
- Identify your 10 mission-critical metrics (readmission rate, length of stay, operating margin, ED wait time)
- Create one certified definition for each, an actual tested SQL query becoming the canonical source
- Implement automated data quality monitoring flagging duplicates and completeness gaps in real-time
- Assign one accountable owner per data domain
- Publish a simple data quality scorecard updated weekly
A 400-bed Ohio health system implemented this lightweight framework in 8 weeks. Within 6 months, metric agreement across departments reached 98%.
According to Gartner’s data quality framework, organizations with formal governance programs report 40% fewer data-related decision errors.
Problem #4: User Access Bottlenecks – Your Warehouse Is a Black Box
The Shadow IT Problem:
Your service line director needs cardiology referral pattern analysis for Thursday’s strategy meeting. She submits an IT ticket Monday morning. Estimated completion: two weeks.
She needs answers in 72 hours. So she exports raw data to Excel, spends 6 hours manually analyzing, and presents results that are probably wrong but “good enough.”
You have dozens of people doing this now. They’ve built shadow analytics ecosystems because your warehouse is theoretically “self-service” but practically requires CCL certification.
The Modern BI Solution:
Layer user-friendly business intelligence platforms on top of your Cerner warehouse, don’t replace it, augment it.
How to Improve Hospital Data Reporting:
Tools like Microsoft Power BI for healthcare and Tableau connect to Cerner databases through standard connectors, providing drag-and-drop interfaces, pre-built healthcare templates, mobile access, and interactive dashboards.
Real Implementation Results:
One 6-hospital health system implemented Power BI:
- Report development time: 3 weeks → 4 hours (91% reduction)
- IT report backlog: Eliminated in 8 weeks
- User adoption: 18% → 67% of target audience
- Shadow spreadsheet systems: Declined 80%
- Implementation cost: $75,000
- Payback period: 6 months
Problem #5: Scaling Failures – When Growth Becomes Your Enemy
Your health system acquires a 150-bed community hospital. Strategically brilliant except your Cerner data warehouse must suddenly ingest their different laboratory system, Epic ambulatory EHR, and separate billing platform.
Your warehouse chokes. ETL jobs fail. Report times triple. Users experience timeouts.
The Fixed Infrastructure Problem:
Legacy on-premises data warehouses have fixed capacity. Adding significant data volume requires capital approval (3-6 months), hardware procurement (2-3 months), and network reconfiguration losing 9-12 months of analytics capability.
Cloud Solves Scaling Permanently:
One health system preparing for ACO expansion needed claims data for 45,000 patients from 7 payers. Their on-premises Cerner warehouse required $600,000 in hardware and 9 months.
Instead, they implemented cloud data lakes using Azure:
- Implementation timeline: 3 weeks to ingest all 7 payer feeds
- Monthly storage cost: $2,400 (versus $600K capital investment)
- Scalability test: When attribution grew to 78,000 patients, accommodation required 2 days and zero infrastructure changes
How to Optimize Cerner Data Warehouse: The Phased Transformation Roadmap
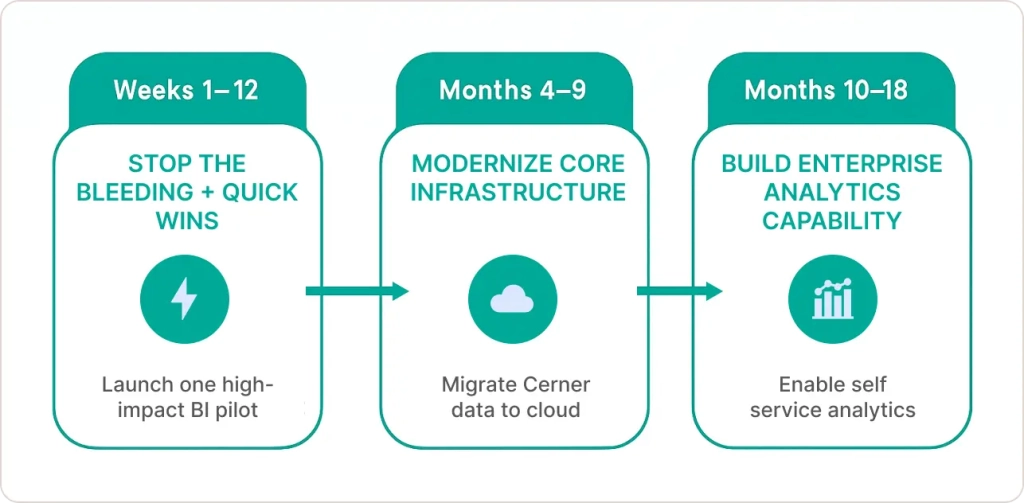
Most consultants pitch 24-month, $5M “digital transformations.” That’s unrealistic and unnecessary.
Here’s what works: phased approaches delivering measurable wins every 90 days that build momentum, prove ROI, and secure funding for subsequent phases.
Phase 1 (Weeks 1-12): Stop the Bleeding + Quick Wins
Goal: Demonstrate warehouse value and build organizational momentum.
Action Items:
- Conduct rapid user needs assessment across clinical, operational, and financial departments
- Select ONE high-impact integration (typically HIE feeds or billing system connection)
- Implement lightweight governance for 10 mission-critical metrics
- Deploy pilot BI tool for one frustrated department (usually finance or quality)
Success Metrics:
- One department reports measurably faster insights (weeks to days)
- IT receives positive feedback instead of complaints
- Pilot users become internal champions
Investment: $50,000-$150,000
ROI Timeline: 4-6 months
Phase 2 (Months 4-9): Modernize Core Infrastructure
Goal: Address architectural bottlenecks compounding performance problems.
Action Items:
- Implement cloud data warehouse (Snowflake, Redshift, Azure Synapse) alongside Cerner
- Replicate Cerner data using change data capture (CDC) for near-real-time sync
- Migrate heavy analytical workloads off production databases
- Expand BI platform to 3-5 departments
Following cerner data warehouse best practices means preserving clinical system stability while optimizing analytics separately.
Success Metrics:
- 10x query performance improvement
- 60% shorter ETL windows
- Eliminated 2 AM IT pages from database timeouts
- User satisfaction increases from 4.2/10 to 7.8/10
Investment: $250,000-$500,000
ROI Timeline: 12-18 months
Phase 3 (Months 10-18): Build Enterprise Capability
Goal: Transform to proactive analytics organization driving strategic value.
Action Items:
- Integrate all major data sources (billing, labs, external claims, SDOH data)
- Implement enterprise master data management solving patient identity permanently
- Roll out self-service analytics organization-wide with training
- Build predictive models for ACO cost drivers
- Establish automated governance monitoring
Success Metrics:
- 60%+ user adoption across organization
- Executive decisions consistently reference data
- Measurable quality and cost improvements
- Zero shadow analytics systems
Investment: $400,000-$800,000 cumulative
Total ROI Timeline: 18-24 months
When to Get Expert Help
You Might DIY Successfully If You Have:
- Data architects who’ve implemented modern cloud warehouses
- BI developers fluent in Power BI or Tableau
- Political capital to enforce governance across departments
- 18-24 months of runway without pressure for immediate results
Get External Help If:
- Your IT team is already underwater
- Previous warehouse improvement initiatives failed
- You need results in under 6 months
- You lack cloud infrastructure expertise
- You want knowledge transfer, not vendor dependency
Real Transformation Example:
A 380-bed Southeast health system engaged us facing $2.8M annual preventable readmission losses, IT spending 40% of time on reports, and ACO contracts at risk.
Our 14-month phased engagement delivered:
- Cloud semantic layer on existing Cerner infrastructure
- Integration of 8 external data sources
- Power BI deployment with 12 pre-built dashboards
- Training for 6 internal analytics champions
Measurable Results:
- 38% reduction in preventable readmissions ($1.1M recovered)
- Report development: 18 days → 3 hours
- User adoption: 71% of staff
- ACO achieved first-time shared savings: $4.2M
Total Investment: $420,000
Year 1 Financial Impact: $4.7M positive
Their internal team now runs everything independently that’s the partnership model that works.
Why This Matters Right Now
Three accelerating factors are creating an unbridgeable gap between data-capable and data-broken health systems:
Factor 1: CMS Quality Penalties Expanding 15% in Q1 2026
New quality measures require health equity data integrating community health information and social determinants tracking. If your warehouse can’t integrate external community data, you face automatic penalties.
You have 8 months. According to CMS quality payment program requirements, hospitals must demonstrate comprehensive data capture capabilities for health equity metrics.
Factor 2: ACO Contract Renewals Demand New Capabilities
Most 2023-2024 ACO contracts had 2-year terms. 2026 renewals require:
- Predictive risk stratification identifying high-cost patients 6 months ahead
- Real-time care gap identification with 24-hour alerts
- Documented closed-loop interventions across settings
- Cross-setting utilization visibility
One CFO lost $3.2M in ACO shared savings because their warehouse couldn’t prove they’d closed care gaps their data showed existed.
Factor 3: Competitors Are Already Using AI
Oracle added generative AI capabilities to Cerner in 2024. But AI trained on garbage data produces garbage predictions.
Health systems with clean, integrated warehouses are deploying predictive models identifying sepsis risk 6 hours earlier, automated prior authorization reducing denials 40%, and NLP extraction pulling social determinants from clinical notes.
The gap between data-capable and data-limited systems isn’t linear, it’s exponential.
The Real Cost Isn’t What You’ve Spent, It’s What You’re Losing Daily
After 50,000+ hours helping health systems transform underperforming analytics platforms, I can tell you with certainty: the infrastructure decisions you make this quarter determine whether your organization can leverage AI, succeed in risk-based contracts, and operate efficiently in an increasingly data-driven industry.
The hospitals winning in 2025 made these investments in 2022-2023 when the ROI wasn’t obvious. They modernized infrastructure when boards questioned urgency. They enforced governance despite resistance. They empowered users despite IT concerns.
Now they’re realizing compounding returns: predictive capabilities preventing costly interventions, operational insights optimizing resource allocation, and clinical intelligence improving outcomes while reducing costs.
Your Warehouse Is Costing You More Than You Think:
The real cost isn’t money spent on underperforming infrastructure. It’s million-dollar strategic decisions being made monthly based on incomplete data that misses 40% of the patient story, delayed insights arriving too late for intervention, conflicting metrics nobody trusts, and lost ACO opportunities because you can’t prove value.
That’s $4.2M annually for the average health system and it’s preventable.
The Transformation Path Forward:
You don’t need a $5M rip-and-replace project. You need focused 90-day initiatives demonstrating value, building momentum, and creating foundation for broader capability development.
Start with Phase 1 quick wins. Expand to Phase 2 infrastructure modernization. Scale to Phase 3 enterprise capabilities.
Ready to diagnose exactly where your Cerner data warehouse is failing and which fixes will deliver ROI fastest? Explore comprehensive healthcare data analytics solutions that maximize value from your existing technology investments, without replacing your entire infrastructure.
The insights your organization needs to thrive already exist in your systems. They just need the right architecture, governance, and tools to surface them effectively.
Don’t let another quarter pass, losing $312,000 monthly to preventable data gaps. The transformation starts with one 90-day phase and the returns compound from there.