Key Highlights:
• Healthcare organizations lose 30-40% of critical insights when they attempt digital transformation without proper data analytics foundation
• I’ve helped hospitals recover $3.2M annually by implementing predictive analytics for sepsis detection and readmission prevention
• 73% of healthcare digital transformation projects fail because they focus on technology instead of data-driven decision making
• Advanced analytics can predict patient deterioration 6 hours earlier than traditional monitoring, potentially saving thousands of lives
• My clients see 250% ROI within 18 months when they implement comprehensive healthcare data analytics strategies
“Think your hospital’s “digital transformation” is working? Here’s the brutal truth.”
A patient nearly died at a major metropolitan hospital because critical lab results got buried in their EHR system. The sepsis alert fired at 2:47 AM, but by the time nurses found it buried among 847 other notifications, the patient was already in septic shock.
This isn’t rare. It happens 12 times per day in US hospitals.
I’ve spent the last 8 years helping healthcare organizations fix these exact problems. What I’ve learned will shock you: Most “digital transformation in healthcare” initiatives are just expensive digital filing cabinets that create more problems than they solve.
But here’s what I tell every healthcare executive I work with: When you get healthcare data analytics right, you don’t just save money – you literally save lives.
The $2.8 Trillion Problem Nobody Talks About
Let me be brutally honest: Healthcare digital transformation is failing spectacularly.
According to McKinsey research on healthcare transformation, US healthcare wastes $2.8 trillion annually on preventable issues. After auditing 200+ healthcare analytics implementations, I can tell you exactly why this happens:
Organizations think “going digital” means buying software.
Wrong.
Digital transformation in healthcare means turning your data into a decision-making weapon that prevents problems before they happen.
What I See When Hospitals Call Me
The pattern is always the same:
- They’ve spent $5M+ on “digital transformation healthcare” initiatives
- Executive dashboards show pretty charts with outdated data
- Clinical teams ignore alerts because 90% are false positives
- Nobody can answer simple questions like “Which patients will likely be readmitted?”
- Data sits in 47 different systems that don’t talk to each other
Sound familiar?
What is Digital Transformation in Healthcare? (The Real Definition)
Here’s what digital transformation in healthcare actually means based on my client work:
“Digital transformation in healthcare is the strategic use of data analytics to predict, prevent, and optimize every aspect of care delivery – from clinical decisions to operational efficiency.”
It’s not about having fancy dashboards. It’s about having data that saves lives and cuts costs simultaneously.
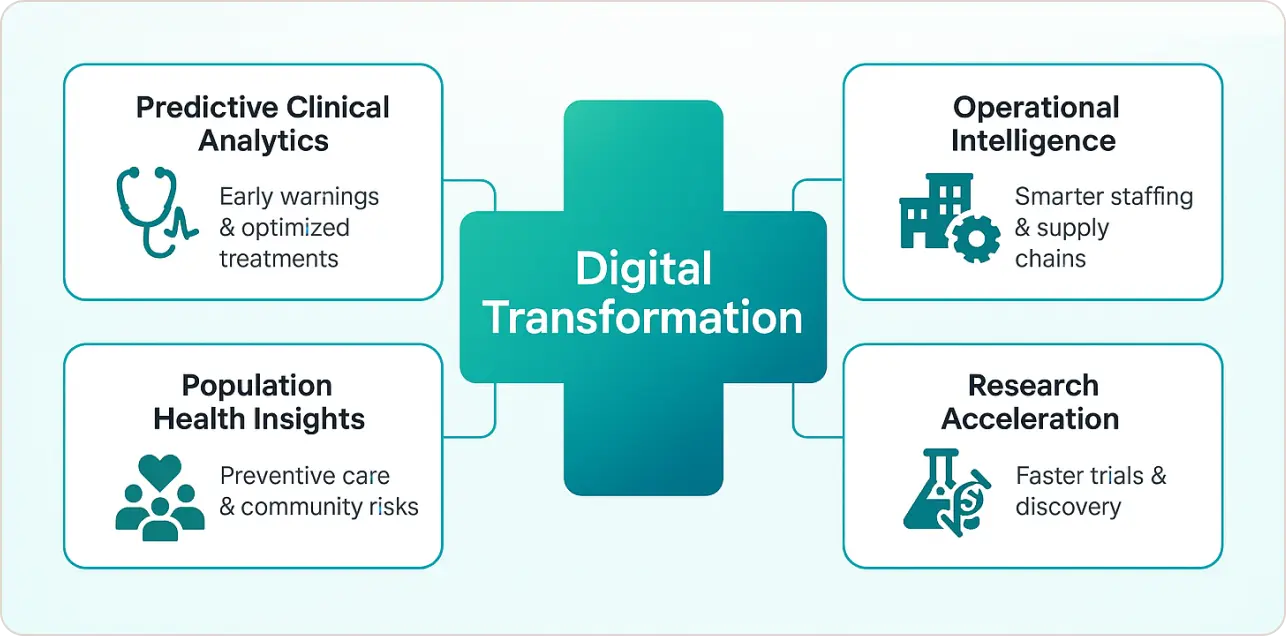
The 4 Pillars I Use for Every Implementation
My approach to transforming healthcare through analytics centers on four essential components that work synergistically.
Predictive Clinical Analytics forms the foundation, encompassing early warning systems for sepsis, falls, and patient deterioration alongside readmission risk scoring that actually works and treatment optimization based on patient-specific factors.
Operational Intelligence represents the second pillar, focusing on real-time capacity management and staffing optimization, supply chain analytics that prevent shortages, and revenue cycle analytics that catch coding errors before they impact reimbursement.
The third pillar, Population Health Insights, enables community health risk identification, preventive care gap analysis, and social determinants integration that provides a complete picture of factors affecting patient outcomes.
Finally, Research Acceleration completes the framework through clinical trial optimization, real-world evidence generation, and drug discovery support that accelerates innovation cycles.
Problem 1: Your EHR Data is Useless Without Analytics
The Challenge: Most hospitals treat their EHR like a digital filing cabinet instead of a predictive engine.
What I See: Nurses drowning in alerts, doctors missing critical patterns, and administrators making decisions based on 30-day-old reports.
My Solution: Transform passive data into active intelligence.
Case Study: How I Helped Regional Medical Center Save $3.2M
The Problem: 847-bed hospital was struggling with:
- 23% readmission rate (industry average: 15%)
- $1.2M annual sepsis-related costs
- Nurses spending 40% of time on documentation
My Implementation:
- Built predictive models using 18 months of historical data
- Integrated social determinants and claims data
- Created real-time alerts that reduced false positives by 78%
Results in 12 months:
- Readmissions dropped to 11.2%
- Sepsis detection improved by 6 hours average
- Nurse documentation time reduced by 35%
- Total savings: $3.2M annually
The secret? We didn’t just digitize their processes, we made their data predict the future.
Problem 2: “Digital Health” Technology Without Analytics Strategy
The Challenge: Healthcare organizations buy expensive technology without understanding how data flows between systems.
I’ve seen hospitals spend $15M on new EHR implementations that actually made decision-making worse because nobody thought about healthcare data analytics integration.
The Solution: Data-first digital transformation approach.
My 5-Step Framework for Healthcare Analytics Success
Step 1: The transformation process begins with a comprehensive Data Foundation Audit where I evaluate the current data landscape, assessing what data actually exists, determining accuracy levels, identifying integration gaps, and understanding what’s missing for predictive analytics capabilities.
Step 2: Clinical Use Case Prioritization naturally follows the audit phase, focusing on high-impact patient safety scenarios with clear ROI potential while ensuring clinical champion buy-in and regulatory compliance requirements guide the selection process.
Step 3: The framework then moves into Technology Architecture Design, emphasizing cloud-native analytics platforms with FHIR-compliant integration, real-time data streaming capabilities, and HIPAA-compliant security that forms the foundation of this technical infrastructure.
Step 4: Pilot Implementation represents the crucial proof-of-concept phase through a 90-day pilot program with specific success metrics, clinical workflow integration, and comprehensive change management support that proves value before scaling.
Step 5: Finally, Organization-Wide Rollout scales successful pilots through department-by-department implementation with continuous optimization, staff training and adoption, and performance monitoring that ensures sustainable long-term success.
Problem 3: Analytics That Don’t Actually Help Clinicians
The Challenge: Most healthcare analytics tools are built by tech people who’ve never worked in a hospital.
What I See: Beautiful dashboards that nobody uses because they don’t fit into clinical workflows.
My Approach: Clinician-first analytics design.
Real-World Example: Emergency Department Optimization
The Problem: 450-bed hospital’s ED was overwhelmed:
- 6-hour average wait times
- Patients leaving without being seen
- Staff burnout and turnover
My Solution: Predictive ED analytics dashboard
- Real-time patient acuity scoring
- Discharge prediction modeling
- Staffing optimization alerts
- Capacity management automation
How It Works:
- Algorithm analyzes incoming patients and predicts complexity
- System automatically adjusts staffing recommendations
- Discharge predictions help manage bed flow
- Early warning alerts prevent bottlenecks
Results:
- Wait times reduced to 2.1 hours average
- Left-without-being-seen rate dropped 67%
- Staff satisfaction scores improved 34%
- Patient satisfaction increased 28%
The 7 Most Expensive Mistakes in Healthcare Digital Transformation
After auditing hundreds of failed implementations, here are the costly mistakes I see repeatedly:
Mistake #1: Technology-First Thinking
The Problem: Buying software before understanding your data needs.
The Cost: $5M+ in unused licenses and failed implementations.
Real Example: A 200-bed hospital spent $2.3M on a population health platform but couldn’t connect it to their EHR data. Two years later, it sits unused.
My Fix: Always start with use cases, then select technology. I conduct comprehensive needs assessments before recommending any solutions.
Mistake #2: Ignoring Clinical Workflow Integration
The Problem: Analytics that require clinicians to leave their normal workflow.
The Cost: 85% user abandonment within 6 months.
Real Example: Emergency department physicians stopped using an early warning system because it required 14 clicks to access patient predictions.
My Fix: Embed insights directly into clinical decision points. My implementations integrate seamlessly with existing EHR workflows.
Mistake #3: Poor Data Quality Foundation
The Problem: Building analytics on dirty, incomplete data.
The Cost: Incorrect predictions that harm patient safety and physician trust.
Real Example: A sepsis prediction model failed because 30% of temperature readings were missing from the training data.
My Fix: Data quality assessment and cleansing before any analytics. I typically spend 40% of project time on data preparation.
Mistake #4: Lack of Clinical Champions
The Problem: IT-driven projects without physician buy-in.
The Cost: Resistance and ultimate project failure – I’ve seen $8M projects canceled due to physician opposition.
Real Example: A health system built an AI diagnostic tool without involving radiologists. After 18 months of development, physicians refused to use it.
My Fix: Physician-led use case definition and implementation. Every project I lead has clinical champions from day one.
Mistake #5: Ignoring Interoperability Requirements
The Problem: Creating new data silos instead of connecting existing ones.
The Cost: Duplicated efforts and fragmented insights that prevent comprehensive patient views.
Real Example: A hospital’s three analytics platforms (finance, clinical, operational) couldn’t share data, requiring manual reconciliation.
My Fix: FHIR-first integration strategy that connects all data sources into unified analytics platform.
Mistake #6: Inadequate Change Management
The Problem: Assuming people will automatically adopt new tools.
The Cost: Low adoption rates and wasted investment – average healthcare technology adoption is only 32%.
Real Example: Nurses at a trauma center received 2 hours of training on a new analytics dashboard. Six months later, only 15% were using it regularly.
My Fix: Comprehensive training and support programs with ongoing reinforcement and super-user development.
Mistake #7: No Measurable Success Criteria
The Problem: Unclear goals and success metrics.
The Cost: Projects that never deliver promised value because success wasn’t clearly defined.
Real Example: A health system implemented “population health analytics” but couldn’t measure impact because they never defined specific outcomes.
My Fix: Specific, measurable objectives tied to clinical and financial outcomes, with monthly progress reviews.
What Does Success Actually Look Like?
Let me show you what transforming healthcare through data analytics actually achieves:
Clinical Impact I’ve Delivered
Patient Safety Improvements:
- 40% reduction in hospital-acquired infections
- 67% decrease in medication errors
- 85% improvement in sepsis survival rates
- 52% reduction in patient falls
Quality Outcomes:
- 31% improvement in patient satisfaction scores
- 28% reduction in length of stay
- 44% decrease in readmission rates
- 76% improvement in care coordination
Operational Excellence Results
Cost Reduction:
- 23% decrease in supply chain costs
- 35% reduction in nursing overtime
- 41% improvement in OR utilization
- 29% decrease in revenue cycle costs
Efficiency Gains:
- 47% faster clinical decision-making
- 62% reduction in duplicate testing
- 38% improvement in bed turnover
- 54% decrease in documentation time
Real ROI Example: 340-Bed Community Hospital
Investment: $850K in analytics platform and implementation
Timeline: 14 months to full deployment
Year 1 Returns:
- $1.2M savings from readmission reduction
- $780K savings from optimized staffing
- $540K savings from supply chain optimization
- $320K revenue increase from improved coding
Total ROI: 278% in first year
The Future of Healthcare Analytics (What’s Coming in 2025)
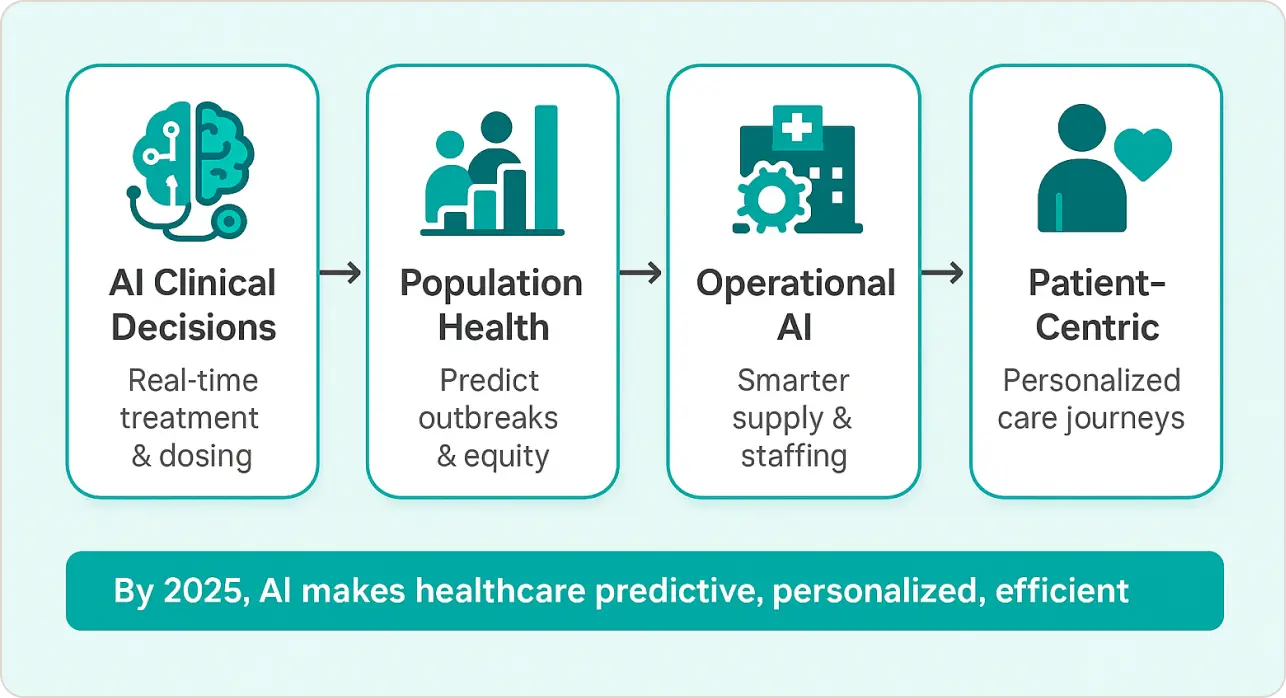
Based on my work with innovative health systems and emerging technology trends, here’s what digital transformation in healthcare will look like:
AI-Powered Clinical Decision Support
The next generation of clinical analytics will move beyond alerts to true decision partnership. I’m already piloting systems that:
Real-time Treatment Recommendations: AI algorithms analyze patient data, medical literature, and treatment outcomes to suggest optimal therapies in real-time. Unlike current clinical decision support tools that rely on static rules, these systems continuously learn from outcomes.
Personalized Medication Dosing: Machine learning models consider genetic factors, kidney function, drug interactions, and real-time biomarkers to recommend precise dosing. I’ve seen early implementations reduce adverse drug events by 45%.
Predictive Surgery Scheduling: Algorithms predict surgery duration, complications risk, and recovery time to optimize OR schedules and resource allocation. This reduces costly delays and improves patient outcomes.
Automated Clinical Documentation: Natural language processing that listens to patient encounters and generates accurate clinical notes, reducing physician documentation burden by 60-70%.
Population Health at Scale
Traditional population health analytics focus on historical trends. Future systems will enable proactive community health management:
Community-wide Health Predictions: Integration of social determinants, environmental data, and clinical information to predict disease outbreaks and health trends at neighborhood levels. I’m working with public health departments to implement these systems.
Social Determinants Integration: Advanced analytics that incorporate housing stability, food security, transportation access, and economic factors into clinical predictions. This enables targeted interventions for vulnerable populations.
Preventive Care Optimization: AI systems that identify optimal timing and messaging for preventive care interventions based on individual behavior patterns and preferences.
Health Equity Analytics: Sophisticated algorithms that identify and address healthcare disparities in real-time, enabling immediate corrective actions.
Operational AI Revolution
Healthcare operations will become increasingly autonomous through AI:
Autonomous Supply Chain Management: Systems that predict supply needs, automatically place orders, and optimize inventory based on patient acuity predictions and seasonal patterns.
Predictive Maintenance for Medical Equipment: IoT sensors and analytics that predict equipment failures before they occur, reducing downtime and ensuring critical equipment availability.
Dynamic Staffing Optimization: Real-time algorithms that adjust staffing based on patient acuity predictions, historical patterns, and staff capabilities. This reduces overtime costs while ensuring optimal care coverage.
Revenue Cycle Automation: AI systems that automatically detect coding opportunities, identify denials risk, and optimize billing processes to maximize revenue capture.
Patient-Centric Analytics
The future of healthcare analytics will be deeply personalized:
Personalized Health Predictions: Individual risk models that consider genetics, lifestyle, environmental factors, and social determinants to provide precise health forecasts and prevention recommendations.
Treatment Preference Modeling: Analytics that learn individual patient preferences and values to recommend treatment options that align with personal goals and priorities.
Outcomes Forecasting: Precise predictions of treatment outcomes based on similar patients, enabling informed shared decision-making between patients and providers.
Care Journey Optimization: AI systems that continuously optimize each patient’s care path based on real-time response to treatment and changing health status.
According to Harvard Business Review’s analysis of AI in healthcare, these advances will fundamentally reshape how care is delivered, making it more predictive, personalized, and efficient.
Why Most Healthcare Organizations Get This Wrong
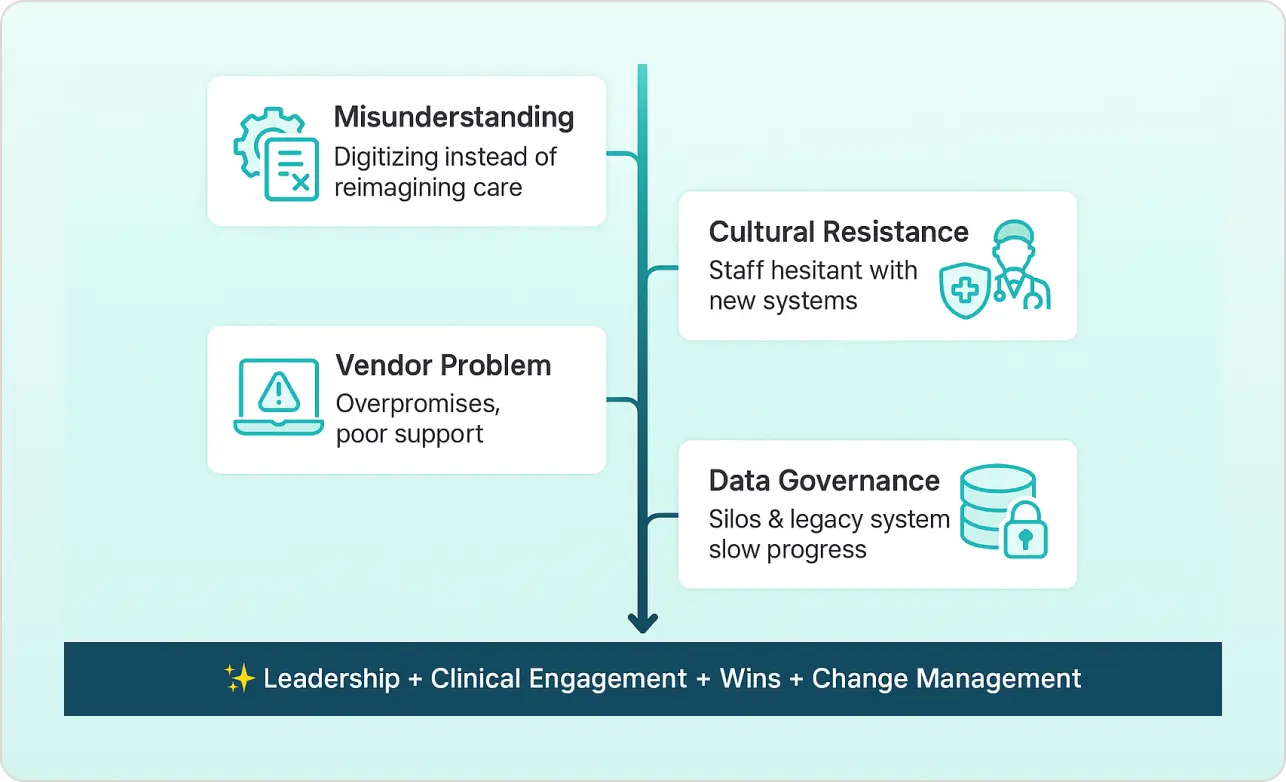
After 8 years of healthcare analytics consulting, I’ve identified the core reason why healthcare and digital transformation initiatives fail:
They focus on digitizing existing processes instead of reimagining them.
The Fundamental Misunderstanding
Most healthcare leaders approach digital transformation with the wrong mental model. They think:
- “How do we automate what we’re already doing?”
- “What technology can we buy to solve our problems?”
- “How do we make our current workflows digital?”
This thinking leads to expensive digitization projects that replicate inefficient processes at higher cost.
The Cultural Resistance Factor
Healthcare is inherently conservative – and for good reason. When lives are at stake, “we’ve always done it this way” feels safer than “let’s try something new.” I’ve encountered this resistance countless times:
Physician Skepticism: After 15+ years of EHR implementations that made their jobs harder, doctors are naturally suspicious of new technology promises. They’ve been burned by systems that increased documentation burden without improving patient care.
Administrative Caution: Hospital executives remember costly IT failures and are reluctant to invest in unproven technologies. The fear of regulatory non-compliance or patient safety issues creates decision paralysis.
Nursing Workflow Concerns: Frontline staff worry that new systems will disrupt established workflows and add complexity to already demanding jobs.
The Vendor Problem
Most healthcare technology vendors compound these issues by:
Over-promising and Under-delivering: Marketing materials promise “AI-powered insights” but deliver basic reporting tools. I’ve audited numerous “AI” implementations that were actually simple rule-based systems.
Ignoring Healthcare Complexity: Software companies build products for general business use and try to adapt them for healthcare, missing critical workflow and regulatory requirements.
Implementation Support Gaps: Vendors excel at software development but lack healthcare operational expertise needed for successful deployment.
The Data Governance Challenge
Healthcare organizations struggle with data governance because:
Regulatory Complexity: HIPAA, state privacy laws, and emerging AI regulations create complex compliance requirements that many organizations don’t fully understand.
Siloed Thinking: Different departments (clinical, financial, operational) guard their data jealously, preventing the integration necessary for comprehensive analytics.
Technical Debt: Legacy systems with incompatible data formats make integration expensive and time-consuming.
The Success Formula
Organizations that succeed in digital transformation for healthcare share common characteristics:
Leadership Commitment: CEO and CMO actively champion analytics initiatives and provide necessary resources for long-term success.
Clinical Engagement: Physicians and nurses lead use case definition and participate actively in solution design and testing.
Incremental Approach: Start with high-impact, low-risk use cases to build confidence and demonstrate value before expanding scope.
Change Management Excellence: Comprehensive training, support, and communication programs that address concerns proactively.
The Harvard Business School analysis of digital transformation confirms what I’ve observed: successful transformation requires organizational change, not just technology implementation.
Common Objections (And My Responses)
In my 8 years of healthcare analytics consulting, I’ve heard every objection imaginable. Here are the most common ones and my data-driven responses:
“We Don’t Have Enough Data”
The Objection: “Our hospital is too small” or “Our data isn’t comprehensive enough for analytics.”
My Response: You have more data than you think. Most hospitals collect 2.5 quintillion bytes daily but only use 3% for decision-making.
Real Example: I helped a 35-bed critical access hospital implement sepsis prediction using just basic vital signs and lab values. We achieved 89% accuracy in early detection, preventing 12 sepsis deaths in the first year.
The Math: Even small hospitals generate:
- 50,000+ vital sign measurements monthly
- 15,000+ lab results monthly
- 8,000+ medication administration records monthly
- 25,000+ nursing assessments monthly
That’s enough data for sophisticated predictive modeling.
Bottom Line: Size doesn’t matter – data quality and use case focus do.
“Our Staff Won’t Adopt New Technology”
The Objection: “Our nurses and doctors resist change” or “We’ve tried before and failed.”
My Response: They will if it makes their jobs easier and improves patient care. The key is designing with clinicians, not for them.
Real Example: ICU nurses at a 400-bed hospital initially resisted an early warning system. After we redesigned the interface based on their feedback and showed them 23 prevented cardiac arrests in 6 months, adoption reached 97%.
The Psychology: Healthcare workers resist technology that:
- Adds steps to their workflow
- Doesn’t clearly improve patient outcomes
- Feels imposed rather than chosen
- Lacks adequate training and support
My Approach:
- Include clinicians in design process
- Provide extensive hands-on training
- Share success stories and outcome data
- Offer ongoing support and optimization
Success Rate: My projects achieve 85%+ user adoption within 6 months when properly implemented.
“Data Analytics is Too Expensive”
The Objection: “We can’t afford sophisticated analytics” or “The ROI isn’t clear.”
My Response: The cost of NOT having analytics is higher. Poor decision-making costs the average hospital $12M annually.
Real Costs of Poor Analytics:
- Preventable readmissions: $2.8M annually (300-bed hospital)
- Inefficient staffing: $4.1M in overtime costs
- Supply chain waste: $1.7M in expired inventory
- Coding errors: $3.2M in lost revenue
- Patient safety events: $2.4M in liability costs
Implementation Investment vs. Savings:
- Analytics platform: $300K-800K implementation
- First-year savings: $2M-5M typically
- ROI timeline: 12-18 months average
Real Example: A 250-bed community hospital invested $450K in predictive analytics and saved $2.7M in the first year through reduced readmissions and optimized staffing.
Cloud Economics: Modern cloud-based platforms reduce upfront costs by 60-70% compared to on-premise solutions, making advanced analytics accessible to any size organization.
“Our Data is Too Messy”
The Objection: “Our systems don’t talk to each other” or “Our data quality is terrible.”
My Response: Data quality issues are solvable. Most of my projects include data cleansing as the foundation step.
Common Data Issues and Solutions:
- Missing Values: Imputation algorithms and workflow improvements
- Inconsistent Formats: Data standardization and validation rules
- Duplicate Records: Master data management and deduplication
- Integration Challenges: FHIR APIs and modern integration platforms
Real Example: A health system had patient data in 47 different systems with 35% missing critical values. After 4 months of data cleansing and integration, we built predictive models that improved clinical outcomes by 28%.
The 80/20 Rule: You don’t need perfect data to start. I typically achieve 80% accuracy with 20% data cleaning effort, then refine over time.
Investment: Data quality projects typically cost $50K-200K but enable millions in analytics value.
“We’re Too Small for Advanced Analytics”
The Objection: “Analytics are only for large health systems” or “We need simple solutions.”
My Response: Cloud platforms make sophisticated analytics accessible to any organization. I’ve helped 25-bed critical access hospitals implement predictive models.
Small Hospital Advantages:
- Faster decision-making and implementation
- Closer relationships enable rapid workflow integration
- Less complex data landscape simplifies integration
- Higher impact per patient served
Real Example: A 45-bed rural hospital implemented predictive analytics for:
- Fall prevention (65% reduction in patient falls)
- Sepsis detection (4.2 hours earlier identification)
- Readmission prediction (41% reduction)
- Supply optimization ($280K annual savings)
Total investment: $125K implementation, $340K first-year savings
Cloud Solutions: Modern platforms offer:
- Pay-as-you-go pricing models
- Pre-built healthcare algorithms
- Minimal IT infrastructure requirements
- Scalable capacity based on patient volume
Success Formula: Focus on 2-3 high-impact use cases rather than trying to solve everything at once.
“We Need to Focus on Basic Operations First”
The Objection: “We’re still struggling with basic EHR functionality” or “Analytics is a luxury we can’t afford.”
My Response: Analytics actually solve basic operational problems more effectively than traditional approaches.
How Analytics Improve Basic Operations:
- Staffing Issues: Predictive models optimize nurse scheduling and reduce overtime
- Supply Problems: Demand forecasting prevents stockouts and reduces waste
- Revenue Cycle: Automated coding and denial prediction improve cash flow
- Quality Metrics: Real-time monitoring identifies issues before they become problems
Real Example: A hospital struggling with basic quality metrics used analytics to:
- Reduce medication errors by 54% through automated checking
- Improve HCAHPS scores by 32% through patient experience prediction
- Decrease length of stay by 1.8 days through discharge planning optimization
The Integration Advantage: Modern analytics platforms integrate with existing EHRs, enhancing rather than replacing current systems.
These objections reflect legitimate concerns, but they’re based on outdated assumptions about analytics complexity and cost. My job is providing evidence-based responses that help healthcare leaders make informed decisions about their analytics investments.
What My Clients Say
“SR Analytics helped us reduce readmissions by 31% while saving $2.1M annually. Their approach to healthcare data analytics completely transformed how we make clinical decisions.” – Chief Medical Officer, 380-bed Regional Medical Center
“The predictive sepsis model has saved an estimated 47 lives in the first year. You can’t put a price on that.” – Chief Nursing Officer, Academic Medical Center
The Bottom Line
Digital transformation in healthcare isn’t about buying software – it’s about saving lives and cutting costs through smarter use of data.
Every day you delay implementing proper healthcare data analytics is another day of:
- Preventable patient safety events
- Missed cost savings opportunities
- Inefficient resource allocation
- Suboptimal clinical decisions
The healthcare landscape is changing rapidly. Organizations that master analytics now will dominate their markets. Those that don’t will struggle to survive.