TL;DR
Healthcare AI consulting bridges the gap between AI tools and real hospital operations. Without specialized guidance, hospitals routinely waste $200K to $500K on pilots that never make it through compliance review, EHR integration, or clinical adoption.
A proven path looks like this:
- Start with maturity and data readiness
- Pick one high-ROI low-risk use case
- Build the right architecture (often RAG-based) to reduce hallucinations
- Deploy in phases with governance, training, and monitoring
- Expect break-even by month 12–18 for many programs and 200–300% ROI by year two when executed well
Hospitals don’t fail at AI because they lack ambition. They fail because healthcare is where “cool demo” goes to die.
The technology isn’t the problem. The gap between “AI that impresses venture capitalists” and “AI that survives Epic integration, HIPAA audit, and actual clinical use” is where projects die.
That gap is exactly why healthcare AI consulting exists.
This guide walks through how hospitals move from “we have an AI pilot” to “we have a production system delivering measurable ROI,” typically in 12 to 18 months, without getting crushed by compliance, integration, or clinical rejection.
Quick Answer
Before: Hospitals spend hundreds of thousands on pilots that die in compliance, integration, or adoption.
After: Healthcare AI consulting navigates HIPAA, EHR complexity, FDA considerations, and change management to deliver production-ready systems with measurable ROI.
I’ve seen the same pattern repeat for years:
- The hospital buys cloud and “AI capabilities”
- A data science team builds an impressive demo
- Compliance shuts it down or delays it for months
- Clinicians don’t trust it or won’t use it
- Leadership calls it “not ready” and moves on
The tech rarely fails. The operational reality does.
What Is Healthcare AI Consulting? (And Why Your IT Team Can’t Do This)
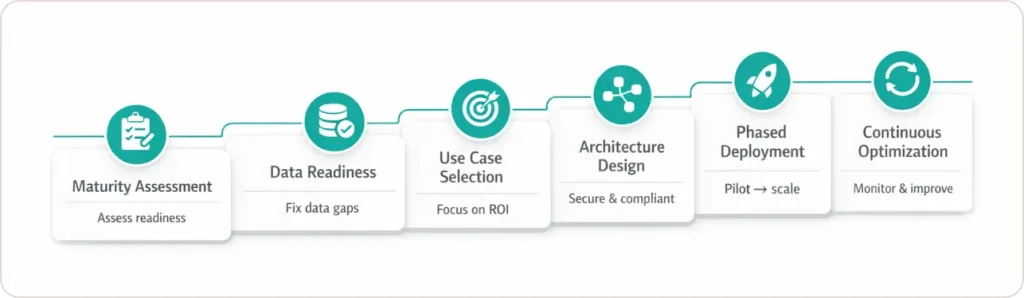
Healthcare AI consulting helps medical organizations implement production-ready artificial intelligence by managing six critical phases: maturity assessment, data readiness validation, use case prioritization, technical architecture design, phased deployment, and continuous optimization.
Here’s what that actually looks like at a 300-bed hospital:
Week 1-2: Consultants audit your current state. They discover your patient data lives in seven systems that don’t talk to each other. Your “data lake” is actually Excel files emailed between departments. Your compliance team has never approved an AI project.
Week 3-6: They build a realistic roadmap. Not “AI everything in 90 days” but “billing automation first (low risk, high ROI), then documentation AI (once we prove value), then clinical decision support (once physicians trust it).”
Months 2-6: They handle the painful middleware work connecting AI to Epic without breaking anything. They write the HIPAA compliance documentation your legal team demands. They train staff who think AI will replace them.
Month 6-18: They deploy in phases, measure actual results, optimize based on real usage, and prevent the model drift that makes AI accuracy decay over time.
Why most internal teams struggle:
Even excellent IT teams often have deep cloud skills but limited healthcare interoperability experience (HL7, FHIR), plus they’re already overloaded running core systems.
Also, hiring internal AI leaders is expensive and slow. And even with talent, first-time implementations fail a lot because clinical workflow adoption can’t be learned from a course. It’s learned through painful mistakes.
Gartner’s 2024 healthcare AI research indicates that organizations with structured, specialist-led AI programs move to production significantly faster and at lower long‑term cost than ad hoc internal efforts.
Why 71% of Hospitals Have AI But 44% Can’t Use It
Many hospitals have some form of AI in or around the EHR.
The problem is the last mile. The part where the AI must survive:
- Compliance review
- Real integration
- Real workflows
- Real humans
The barrier isn’t technology availability. It’s the “last-mile problem.”
The Three Walls That Kill AI Projects
Wall #1: The Compliance Gauntlet
Your data science team builds an AI model that predicts sepsis risk with 94% accuracy. Impressive. Then compliance asks:
- “How do you ensure HIPAA compliance when the model processes PHI?”
- “What’s your FDA registration strategy since this influences clinical decisions?”
- “Show me the bias audit proving this doesn’t discriminate by race or socioeconomic status.”
- “Where’s the documentation proving you can explain every AI decision to a plaintiff’s attorney?”
Silence. Project cancelled.
Wall #2: The Epic Integration Nightmare
Making an LLM read Epic data isn’t a simple API call.
In practice, it’s:
- Fragmented patient data across many tables and systems
- Different workflows across departments and facilities
- Data standards are inconsistently followed
- Connectivity and authentication challenges
- Reliability requirements that don’t exist in normal software projects
This is where AI healthcare consulting becomes critical—bridging technical capability with regulatory requirements and clinical workflow understanding.
Wall #3: The Clinical Adoption Gap
Even if the tech works, clinical adoption can still fail.
To get adoption, you typically need:
- Workflow shadowing
- Interface iteration based on real feedback
- Champions inside clinical teams
- Training and support
- Clear fallback procedures for low-confidence outputs
Technology worked perfectly. Adoption strategy made it valuable.
80% of healthcare AI initiatives fail due to strategy-execution misalignment, not technical limitations alone or 82% cite change management as the top AI failure risk.
How Healthcare AI Consulting Differs From General AI Consulting
AI consulting for healthcare requires specialized expertise in regulatory compliance, data sensitivity protocols, and clinical workflow integration that general AI consultants fundamentally lack.
| Dimension | General AI Consulting | Healthcare AI Consulting | Internal AI Team |
|---|---|---|---|
| Regulatory Expertise | Data protection basics | HIPAA, FDA, state laws, ethics boards | Must hire compliance specialists |
| Implementation Timeline | 3-6 months typical | 12-18 months for clinical systems | 18-24 months learning curve |
| Upfront Investment | $100K-300K | $200K-500K mid-sized projects | $500K+ annual salaries |
| Success Rate | 60-70% reach production | 85-90% with specialized consultants | 30-40% for first attempts |
| Risk Profile | Revenue loss, inefficiency | Patient safety, regulatory penalties, malpractice | Same risks plus opportunity cost |
Which AI Bet Should You Make First? (The Use Case Priority Matrix)
The Winning Move: Revenue Cycle Automation First
Pick ONE high-ROI, low-risk use case that delivers visible results in 90 days. Usually, that’s revenue cycle automation (insurance verification, medical coding, claims management) because:
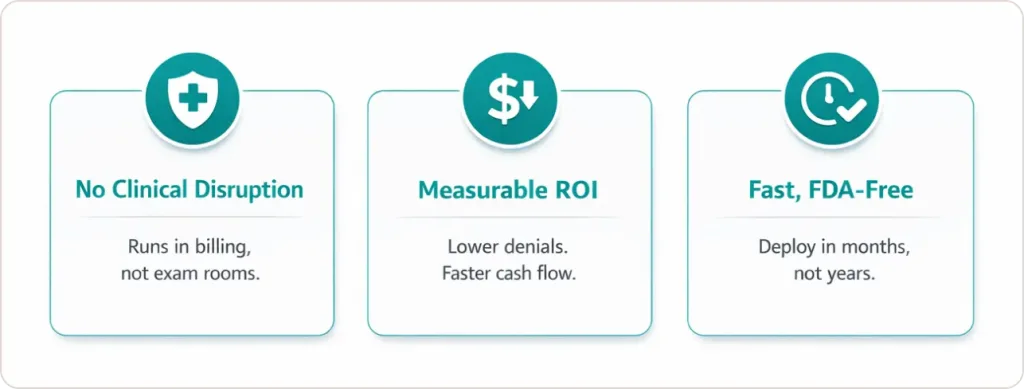
Advantage #1: No Clinical Workflow Disruption
Revenue cycle AI works in billing departments, not exam rooms. You don’t need physician buy-in. You don’t risk patient safety. You don’t trigger clinical resistance.
Advantage #2: Measurable Financial Results
Claim denial rates drop 30%. Discharged-not-final-billed cases decrease 50%. Days in accounts receivable shrink by 15. Finance sees ROI in dollars, not abstract “efficiency gains.”
Advantage #3: Fast FDA-Free Implementation
Revenue cycle AI doesn’t influence clinical decisions, so it avoids FDA medical device classification. Implementation takes 3-6 months instead of 12-18 months.
Real-World Proof:
- Auburn Community Hospital: Revenue cycle AI reduced discharged-not-final-billed cases by 50%, directly improving cash flow
- The Therapy Network: EHR-RCM AI platform saved $79,000 in 3 months with 33% reduction in claim denials
- New York Hospital System: Discharge coordination AI avoided $1.5M in annual CMS readmission penalties
Once finance sees ROI, clinical AI projects get funded. Use billing success as proof-of-concept for everything else.
The Second Wave: Clinical Documentation AI
After proving AI value in billing, tackle the problem burning out every physician: documentation.
This is where you can reduce clinician burden and improve:
- Provider satisfaction
- Patient throughput
- Coding completeness
- Revenue capture
Documentation AI also builds trust because clinicians feel the benefit directly.
Penn Highlands Healthcare Success: Integrated AI assistant decreased documentation time by 2 hours daily per provider. Result: $7 million revenue boost from increased patient capacity plus improved provider satisfaction scores. (Source)
The Third Wave: Clinical Decision Support
Only after proving ROI in billing and documentation should you attempt clinical decision support AI. Why wait?
- Highest regulatory scrutiny (FDA oversight, liability concerns)
- Complex integration (real-time EHR data, lab systems, imaging archives)
- Clinical skepticism (physicians trust AI only after seeing value elsewhere)
- Longest deployment timeline (12-18 months, including validation, training, and change management)
“The potential for AI to transform healthcare is enormous, but implementation requires starting with use cases that demonstrate clear value and build trust across the organization.” — Dr. David Bates, MD, MSc, Chief of General Internal Medicine, Brigham and Women’s Hospital, Professor of Medicine, Harvard Medical School [Source]
What Healthcare AI Consulting Actually Costs (And What You Get)
Pricing varies widely based on scope, readiness, and risk profile. But most programs fall into predictable bands.
Typical Investment Ranges
| Service Tier | Cost Range | Timeline | What You Actually Receive |
|---|---|---|---|
| Maturity Assessment | $50K-$75K | 2-4 weeks | Gap analysis, readiness score, prioritized roadmap, ROI projections |
| Strategy Development | $75K-$150K | 4-8 weeks | Technical architecture design, vendor selection, governance framework, implementation plan |
| Single-Department Implementation | $200K-$500K | 6-12 months | Revenue cycle AI OR documentation AI fully deployed with training |
| Multi-Department Rollout | $500K-$1M | 12-18 months | Multiple use cases integrated, complete change management, optimization |
| Enterprise Transformation | $1M-$3M+ | 18-24 months | Hospital-wide AI infrastructure, all clinical and operational use cases |
| Managed Services | $10K-$50K/month | Ongoing | Model monitoring, retraining, compliance updates, performance optimization |
Hidden Costs to Budget For
- Software licenses
- Cloud compute
- Internal staff time (IT + compliance + clinical leadership)
- Training
- Maintenance and monitoring
ROI Reality Check: When Do You Actually Make Money?
Most organizations break even on AI investment. Here’s the typical financial trajectory:

Year 1: Investment Phase Costs exceed benefits, but baseline efficiency gains and small documentation time savings emerge.
Year 2: Value Realization Phase Quantifiable revenue lift, reduced claim denials, increased patient volume, deliver 200-300% ROI.
Year 3: Maturity Phase Sustained margin expansion, competitive advantage, reduced staff turnover, generate 400-500% cumulative ROI.
The key is avoiding “pilot forever.” ROI requires production deployment and adoption.
The Technical Architecture That Actually Works (RAG Systems Explained Simply)
The breakthrough technology making healthcare AI finally reliable is RAG: Retrieval-Augmented Generation. This solves the “hallucination problem” where AI confidently invents false information.
Why Hospital AI Needs RAG Architecture
The Problem:
Standard Large Language Models are trained on general internet data. When asked “What’s the post-op protocol for this patient?”, they generate plausible-sounding answers based on patterns, not your hospital’s actual protocols.
The RAG Solution:
Instead of guessing, RAG-enabled AI retrieves verified information from your specific knowledge bases:
- Your hospital’s clinical protocols
- This patient’s complete medical history
- Current medication interactions database
- Your payer’s coverage policies
The AI then generates responses grounded in your actual data, not generic patterns.
The Five-Layer Technical Stack
Layer 1: Logic and Reasoning Engine
Tools like LangChain or LangGraph orchestrate multi-step queries. Example:
- “Check this patient’s allergy list”
- “Review contraindications for proposed medication”
- “Verify insurance coverage”
- “Generate prior authorization request”
Layer 2: Knowledge Base (Vector Database)
Pinecone, Chroma, or Weaviate store your clinical data as “embeddings” that AI can search efficiently.
Layer 3: Interface Layer
Voice AI, mobile apps, or web portals where clinicians and patients interact—integrated into existing workflows rather than creating parallel systems.
Layer 4: Security and Compliance Gate
Role-Based Access Control (RBAC), encryption (AES-256 standard), HIPAA audit trails, and PHI de-identification.
Layer 5: Legacy System Connector
Middleware bridges AI to Epic, Cerner, and Meditech through FHIR-formatted data translation, authentication management, real-time synchronization, and fallback procedures.
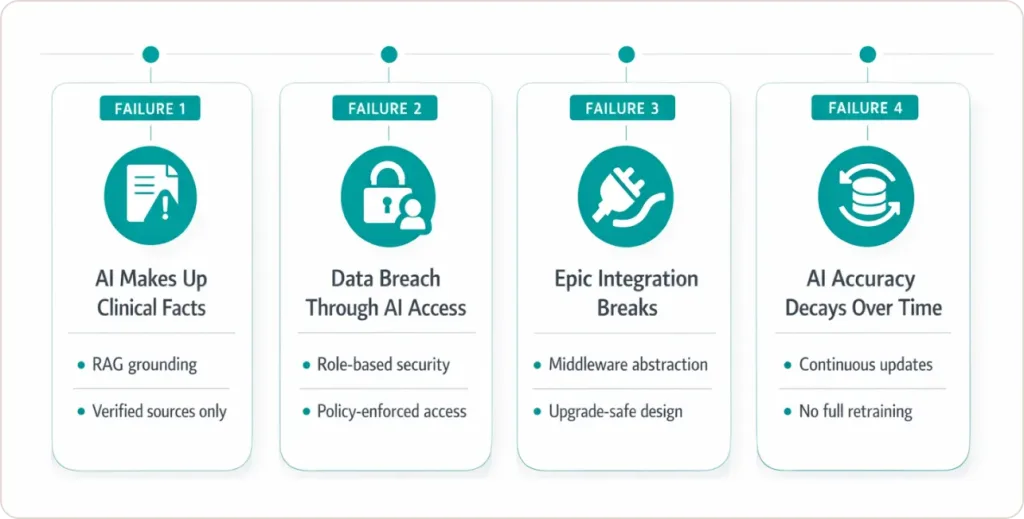
Why This Architecture Prevents the Most Common AI Failures
Failure Mode #1: AI Makes Up Clinical Facts
RAG prevents this by grounding every response in verified source documents. If information doesn’t exist in your knowledge base, AI says “I don’t have that information” instead of inventing answers.
Failure Mode #2: Data Breach Through AI Access
The security layer enforces that AI can only access data that the requesting user is authorized to see. A receptionist’s query can’t retrieve the physician notes.
Failure Mode #3: Epic Integration Breaks
Middleware provides an abstraction layer. When Epic releases updates, you update the middleware instead of rebuilding the entire AI system.
Failure Mode #4: AI Accuracy Decays Over Time
Vector databases allow continuous updates. As protocols change, new information automatically becomes available to AI without retraining entire models.
According to Google Cloud, Retrieval-Augmented Generation (RAG) significantly reduces LLM hallucinations by grounding responses in authoritative sources, while maintaining fast response times for enterprise applications.
| Component | Technology Options | Healthcare-Specific Requirement |
|---|---|---|
| Reasoning Engine | LangChain, LangGraph, Custom | Multi-step clinical decision pathways |
| Vector Database | Pinecone, Chroma, Weaviate | HIPAA-compliant cloud hosting |
| Foundation Model | GPT-4, Claude, Med-PaLM 2 | Medical knowledge pre-training |
| Interface | Voice AI (Nuance), Custom Web/Mobile | Clinical workflow integration |
| Security | Azure Healthcare APIs, AWS HealthLake | BAA-covered, audit logging |
| EHR Connector | FHIR APIs, Custom Middleware | Epic/Cerner certification |
How to Choose Healthcare AI Consultants Who Actually Deliver
The Three Non-Negotiable Qualifications
Qualification #1: Healthcare Regulatory Track Record
Your consultant must have documented experience navigating HIPAA Security Risk Assessments, FDA Pre-Submission Meetings, and Joint Commission Readiness.
The Test Question:
“Walk me through how you’d document our AI system for a HIPAA audit.”
If they give generic compliance answers, walk away. You need someone who’s actually sat through regulatory reviews.
Qualification #2: EHR Integration Battle Scars
Anyone can integrate with APIs in a test environment. Healthcare requires integrating with Epic systems running 15-year-old versions, handling data from acquired hospitals using different EHR vendors, and maintaining performance during 2 AM go-lives.
The Test Question: “Describe your most difficult Epic integration and how you solved it.”
You want to hear about HL7 message failures, authentication nightmares, and data mapping challenges—not theoretical best practices.
Qualification #3: Clinical Change Management Proof
Technology works, but physicians won’t use it = $500K waste. Your consultant needs documented success getting clinicians to adopt new workflows.
The Test Question: “Show me before/after adoption rates from your last three healthcare AI projects.”
Demand actual metrics: percentage of clinicians using the system daily, time to 80% adoption, and reduction in support tickets over time.
The Real Risks Nobody Mentions (And How to Mitigate Them)
AI in healthcare isn’t just “another IT project.” The risk profile is different.
Key risks include:
- Algorithmic bias
- Model drift
- Vendor lock-in
- Compliance breach
- Clinical rejection
Mitigation isn’t optional. It’s part of production readiness.
Healthcare data breaches averaged $9.77M in 2024, the costliest industry again. IBM Cost of a Data Breach Report 2024 [Source]
Where Healthcare AI Consulting Is Heading (What Matters for Your 2025 Decision)
The Agentic AI Wave (Happening Now, Not 2027)
What’s Changing:
Instead of single-purpose AI tools (one for documentation, another for billing, another for imaging), agentic systems orchestrate multiple AI agents that collaborate autonomously.
Example Workflow:
- Intake Agent (voice AI): Gathers patient symptoms and insurance information
- Eligibility Agent: Verifies coverage and identifies authorization requirements
- Clinical Decision Agent: Analyzes symptoms against guidelines and patient history
- Documentation Agent: Generates a structured note from the conversation
- Scheduling Agent: Books follow-up and specialist referrals automatically
- Why This Matters for Your 2025 Buying Decision:
Agentic platforms launching Q2-Q3 2025 may make current point-solution AI investments obsolete within 18 months. Strategic question: Wait for agentic platforms or deploy current RAG systems, knowing migration costs come later?
Microsoft announced agentic AI advancements for healthcare at Ignite 2025, including the Azure AI Foundry Agent Service (now GA) and healthcare-specific orchestrator samples signaling production-ready capabilities for enterprise healthcare partners in 2025.
Conclusion: Making Healthcare AI Work in the Real World
Healthcare AI consulting isn’t about implementing the latest technology trends. It’s about bridging the gap between what’s technically possible and what’s operationally sustainable in complex, highly regulated healthcare environments.
The organizations succeeding with AI share common characteristics: they start with honest maturity assessments, prioritize high-ROI use cases, invest in robust governance frameworks, and recognize that workforce transformation matters as much as technical implementation.
The future of healthcare depends on successfully operationalizing AI at scale. That requires more than software licenses—it requires strategic consulting that addresses the full complexity of clinical workflows, regulatory compliance, and organizational change.